The gut-liver-brain axis is a three-way highway of information interaction among the gastrointestinal tract, liver, and nervous systems. In the past few decades, breakthrough progress has been made in this axis, mainly through understanding its formation mechanism and increasing treatment strategies.
Source: Gut liver brain axis in diseases: the implications for therapeutic interventions, Signal Transduction and Targeted Therapy, by Mengyao Yan, Shuli Man, Benyue Sun, Long Ma, Lanping Guo, Luqi Huang & Wenyuan Gao
The gut-liver-brain axis, a multifaceted network of communication, intricately connects the enteric, hepatic, and central nervous systems [1,2]. One crucial aspect of this complex interaction is the impact of the brain on the functions of the intestines and liver, specifically in relation to the modulation of immune cell activities [3]. On the other hand, the gastrointestinal tract and liver have substantial impacts on cognitive function and overall mental health, primarily by influencing the composition of microbiota and regulating innate immune responses [2].
Source: The Gut-Liver-Brain Axis: From the Head to the Feet, International Journal of Molecular Science, by Mauro Giuffrè and Rita Moretti
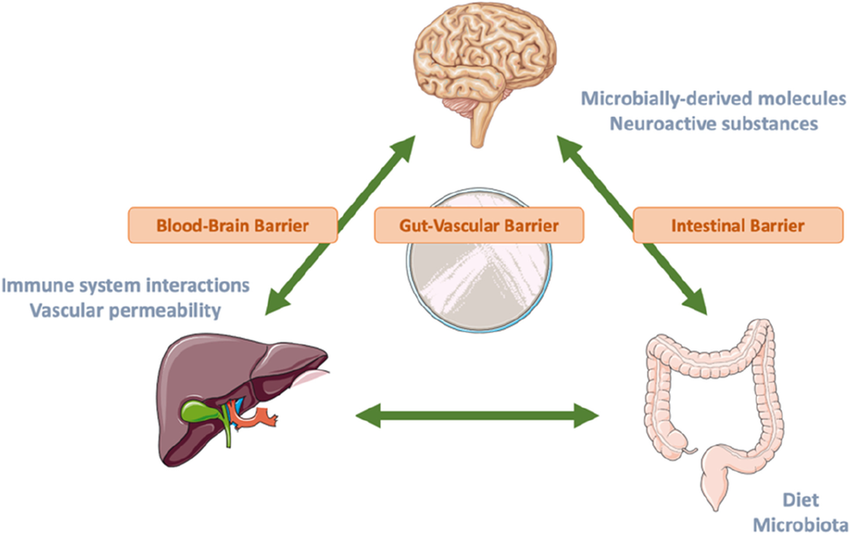
The gut-liver-brain axis describes the bidirectional interaction between the gastrointestinal system, the liver, and the central nervous system with involvement of the gut microbiota. Regulated by the intestinal, blood–brain and gut-vascular barrier, the immune system, and the microbially derived molecules that are derived from diet, the nutrition-gut-liver-brain axis has an essential role in a number of diseases. This review will canvass some of the concepts regarding the nutrition-gut-liver-brain axis and focus on common diseases with recent evidence.
Source: Nutrition and the Gut-Liver-Brain Axis, Current Hepatology Reports, by Agnes H. Y. Ho, Sunny Wong, and Rashid N Lui
The gut-brain axis is a bidirectional information interaction system between the central nervous system (CNS) and the gastrointestinal tract, in which gut microbiota plays a key role. The gut microbiota forms a complex network with the enteric nervous system, the autonomic nervous system, and the neuroendocrine and neuroimmunity of the CNS, which is called the microbiota-gut-brain axis. Due to the close anatomical and functional interaction of the gut-liver axis, the microbiota-gut-liver-brain axis has attracted increased attention in recent years. The microbiota-gut-liver-brain axis mediates the occurrence and development of many diseases, and it offers a direction for the research of disease treatment.
Source: Role of gut microbiota via the gut-liver-brain axis in digestive diseases, World Journal of Gastroenterology, by Jian-Hong Ding, Zhe Jin, Xiao-Xu Yang, Jun Lou, Wei-Xi Shan, Yan-Xia Hu, Qian Du, Qiu-Shi Liao, Rui Xie, and Jing-Yu Xu
The liver plays a central role in digestion, metabolism, and immune protection from pathogens (Kalra et al., 2022). Chronic liver disease caused by various etiologies, including viral, metabolic, and autoimmune diseases can impact liver function leading to chronic injury and ultimately liver cirrhosis. The impact of chronic liver injury extends beyond local organ dysfunction, and can cause perturbations systemically affecting extrahepatic organs including the brain (Montano-Loza et al., 2012; Albillos et al., 2014; Liu et al., 2022). This liver-brain interaction can be readily observed in patients who develop hepatic encephalopathy (HE) as a complication of end stage liver disease or liver cirrhosis. Although the pathophysiology of HE is incompletely understood, it is thought that alterations in central nervous system blood flow, accumulation of neurotoxic compounds, presence of inflammatory metabolites, and excess bile acids resulting from poor liver function can mediate Central Nervous System (CNS) dysfunction (Rose et al., 2020). Furthermore, symptoms generated from altered brain function, including fatigue, depression, anxiety, sleep disturbance and loss of social interest have been observed in patients with chronic liver conditions with and without cirrhosis and overall have a detrimental effect on patient quality of life (Swain and Jones, 2019). A more granular understanding of the mechanisms governing changes in brain function in relation to liver health will provide a foundation to further develop new diagnostic and therapeutic tools that can be used to improve the care of liver patients afflicted with these debilitating symptoms. The mechanism that links liver health to brain function is thought to be mediated through various avenues within the gut-liver-brain axis (Ding et al., 2020; Blaga et al., 2021; Brescia and Rescigno, 2021; D’Mello and Swain, 2021).
Source: Avenues within the gut-liver-brain axis linking chronic liver disease and symptoms, Frontiers in Neuroscience, by Henry H. Nguyen and Mark G. Swain
The gut-liver-brain axis consists of the complex interplay between the gut–brain, gut–liver, and liver–brain axes, and is a multidirectional communication network that links the enteric, hepatic, and central nervous systems. This communication network has been extended to involve endocrine, humoral, metabolic, and immune routes of communication. Through this network, the brain affects intestinal and hepatic activities, including the activity of innate immune cells and immune effector cells (Teratani et al., 2020). Meanwhile, the gut and liver influence cognition and mental health through the regulation of microbiota and host immune responses. Wang et al. find there was a potential causal relationship between gut microbiota and attention deficit hyperactivity disorder and suggest that the gut bacteria found in this study may reduce the occurrence of attention deficit hyperactivity disorder. Hildenbrand et al. investigate predisposing and precipitating risk factors for delirium (the most common acute neuropsychiatric syndrome in hospitalized patients), and find that delirium in precipitating gastrointestinal and hepato-pancreato-biliary diseases was not associated with higher age per se, but with cognitive and functional impairment. Diet is a modulator of the microbiome and is known to impact the gut-brain axis, including its influence on acute brain injuries. Krakovski et al. show that diets and probiotics beneficially modulate immune and neuronal functions, as well as the therapeutic importance of modulation by diets and probiotics.
Source: Editorial: Gut-liver-brain axis: a complex network influences human health and diseases, Frontiers in Neuroscience by Wu Hongjin, Juehua Yu, and Ming Shi
The gut vascular barrier (GVB) represents the inner layer of defense in the multilayered intestinal barrier system that finely regulates the translocation of substances from the intestinal lumen to the systemic circulation. Alterations in gut microbiota barrier homeostasis can lead to the development of intestinal and extraintestinal disease induced by a leaky gut. Increased GVB permeability can lead to leakage of harmful molecules into the blood circulation, with consequent damage to other organs along the gut–liver–brain axis. Targeting the GVB and the active molecules that drive the vascular connection of the gut–liver–brain axis might provide additional therapeutic approaches to diseases affecting organs other than the intestine.Source: The gut vascular barrier: a new player in the gut–liver–brain axis, Trends in Molecular Medicine, by Paola Brescia and Maria Rescigno.
Recent clinical and experimental evidence has evoked the concept of the gut–brain axis to explain mutual interactions between the central nervous system and gut microbiota that are closely associated with the bidirectional effects of inflammatory bowel disease and central nervous system disorders1,2,3,4. Despite recent advances in our understanding of neuroimmune interactions, it remains unclear how the gut and brain communicate to maintain gut immune homeostasis, including in the induction and maintenance of peripheral regulatory T cells (pTreg cells), and what environmental cues prompt the host to protect itself from development of inflammatory bowel diseases. Here we report a liver–brain–gut neural arc that ensures the proper differentiation and maintenance of pTreg cells in the gut. The hepatic vagal sensory afferent nerves are responsible for indirectly sensing the gut microenvironment and relaying the sensory inputs to the nucleus tractus solitarius of the brainstem, and ultimately to the vagal parasympathetic nerves and enteric neurons. Surgical and chemical perturbation of the vagal sensory afferents at the hepatic afferent level reduced the abundance of colonic pTreg cells; this was attributed to decreased aldehyde dehydrogenase (ALDH) expression and retinoic acid synthesis by intestinal antigen-presenting cells. Activation of muscarinic acetylcholine receptors directly induced ALDH gene expression in both human and mouse colonic antigen-presenting cells, whereas genetic ablation of these receptors abolished the stimulation of antigen-presenting cells in vitro. Disruption of left vagal sensory afferents from the liver to the brainstem in mouse models of colitis reduced the colonic pTreg cell pool, resulting in increased susceptibility to colitis. These results demonstrate that the novel vago-vagal liver–brain–gut reflex arc controls the number of pTreg cells and maintains gut homeostasis. Intervention in this autonomic feedback feedforward system could help in the development of therapeutic strategies to treat or prevent immunological disorders of the gut.
Source: The liver–brain–gut neural arc maintains the Treg cell niche in the gut, Nature, by Toshiaki Teratani, Yohei Mikami, Nobuhiro Nakamoto, Takahiro Suzuki, Yosuke Harada, Koji Okabayashi, Yuya Hagihara, Nobuhito Taniki, Keita Kohno, Shinsuke Shibata, Kentaro Miyamoto, Harumichi Ishigame, Po-Sung Chu, Tomohisa Sujino, Wataru Suda, Masahira Hattori, Minoru Matsui, Takaharu Okada, Hideyuki Okano, Masayuki Inoue, Toshihiko Yada, Yuko Kitagawa, Akihiko Yoshimura, Mamoru Tanida, …Takanori Kanai
The gut–liver–brain axis constitutes a multidirectional communication network that connects the enteric, hepatic, and central nervous systems. Through the complex interplay between the gut–liver, gut–brain, and liver–brain axes, this communication network extends to involve endocrine, immune (humoral), and metabolic routes of communication. Within the network, the gut and liver affect cognitive behaviors through the host’s immune responses and the regulation of microbiota, and the brain also influences intestinal and hepatic activities. Studies in animals have shown that an impaired gut–liver–brain axis is associated with diseases such as hepatic encephalopathy, Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis, depression, and autism spectrum disorder (ASD). Source: The Gut–Liver–Brain Axis, E Scholarly Community Encyclopedia.
Hepatic encephalopathy (HE) is a clinical manifestation of neurological and psychiatric abnormalities that are caused by complications of liver dysfunction including hyperammonemia, hyperuricemia, and portal hypertension. Accumulating evidence suggests that HE could be reversed through therapeutic modifications of gut microbiota. Multiple preclinical and clinical studies have indicated that gut microbiome affects the physiological function of the liver, such as the regulation of metabolism, secretion, and immunity, through the gut-liver crosstalk. In addition, gut microbiota also influences the brain through the gut-brain crosstalk, altering its physiological functions including the regulation of the immune, neuroendocrine, and vagal pathways. Thus, key molecules that are involved in the microbiota-gut-liver-brain axis might be able to serve as clinical biomarkers for early diagnosis of HE, and could be effective therapeutic targets for clinical interventions. In this review, we summarize the pathophysiology of HE and further propose approaches modulating the microbiota-gut-liver-brain axis in order to provide a comprehensive understanding of the prevention and potential clinical treatment for HE with a microbiota-targeted therapy. Source: Microbiota-gut-liver-brain axis and hepatic encephalopathy, Microbiome Research Reports, by Haifeng Lu , Hua Zhang , Zhongwen Wu , and Lanjuan Li
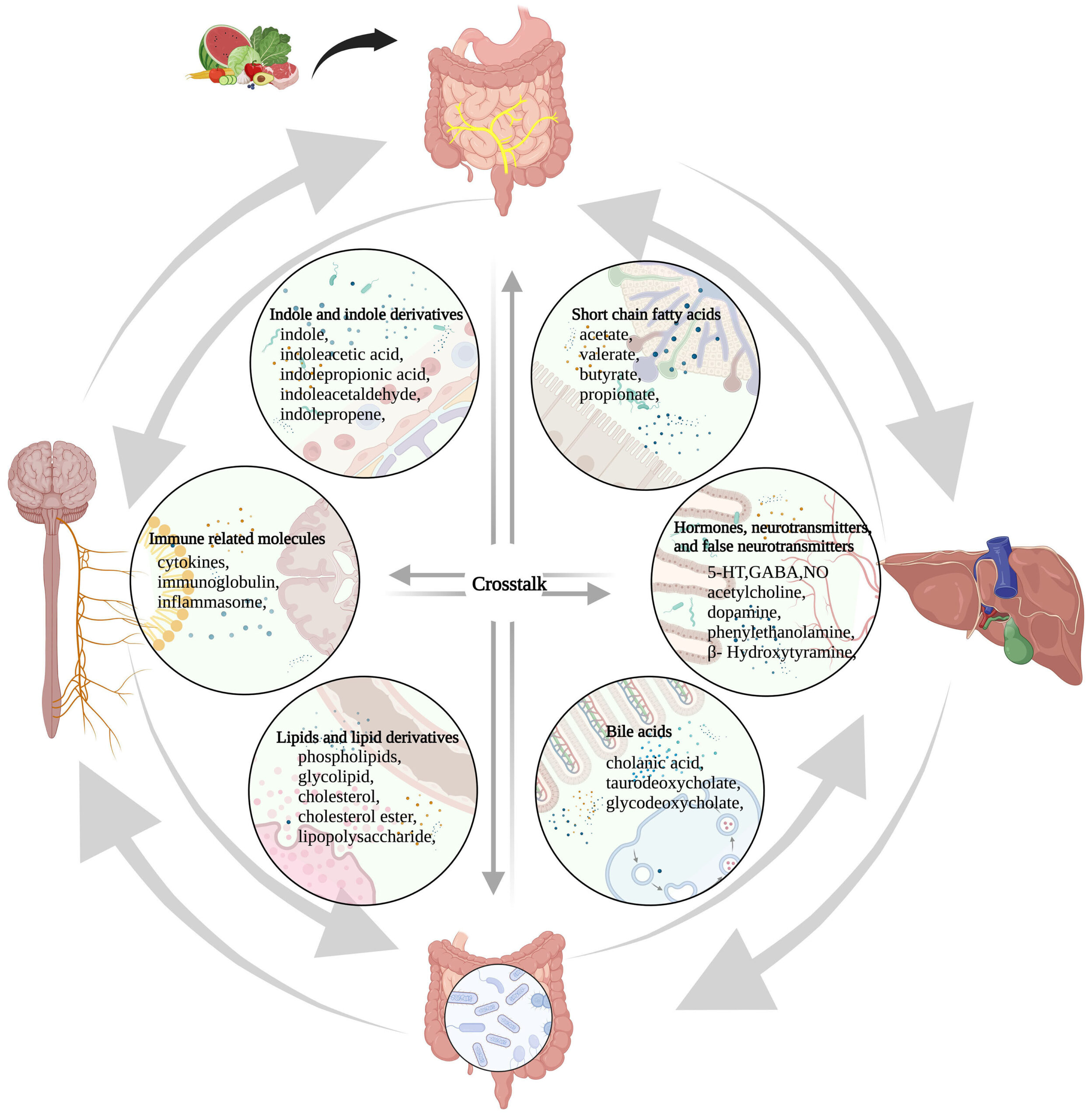
Figure 1. The microbiome-gut-liver-brain axis and molecules involved in this network. These molecules are classified into six categories, including short-chain fatty acids, hormones, neurotransmitters and false neurotransmitters, bile acids, lipids and lipid derivatives, and immune-related molecules, indole and indole derivatives. Amino acids, glucose, protein, fatty acids, vitamins, minerals, and other nutrients that are absorbed from food in the gut participate in the synthesis and conversion of these molecules directly or indirectly. 5-HT: 5-hydroxytryptamine; GABA: γ-aminobutyric acid; NO: nitric oxide.
Source: Microbiota-gut-liver-brain axis and hepatic encephalopathy